Imagine a healthcare system where zip code doesn’t dictate diagnoses, skin color doesn’t predict prognosis, and access to quality care isn’t gated by privilege. This utopian vision may seem distant, but a wave of innovative hospital systems are actively building bridges toward that reality, tackling the entrenched health equity crisis head-on. Let’s delve into their groundbreaking initiatives, unraveling the threads of their success and weaving new possibilities for a more just healthcare landscape.
Boston Medical Center (BMC):
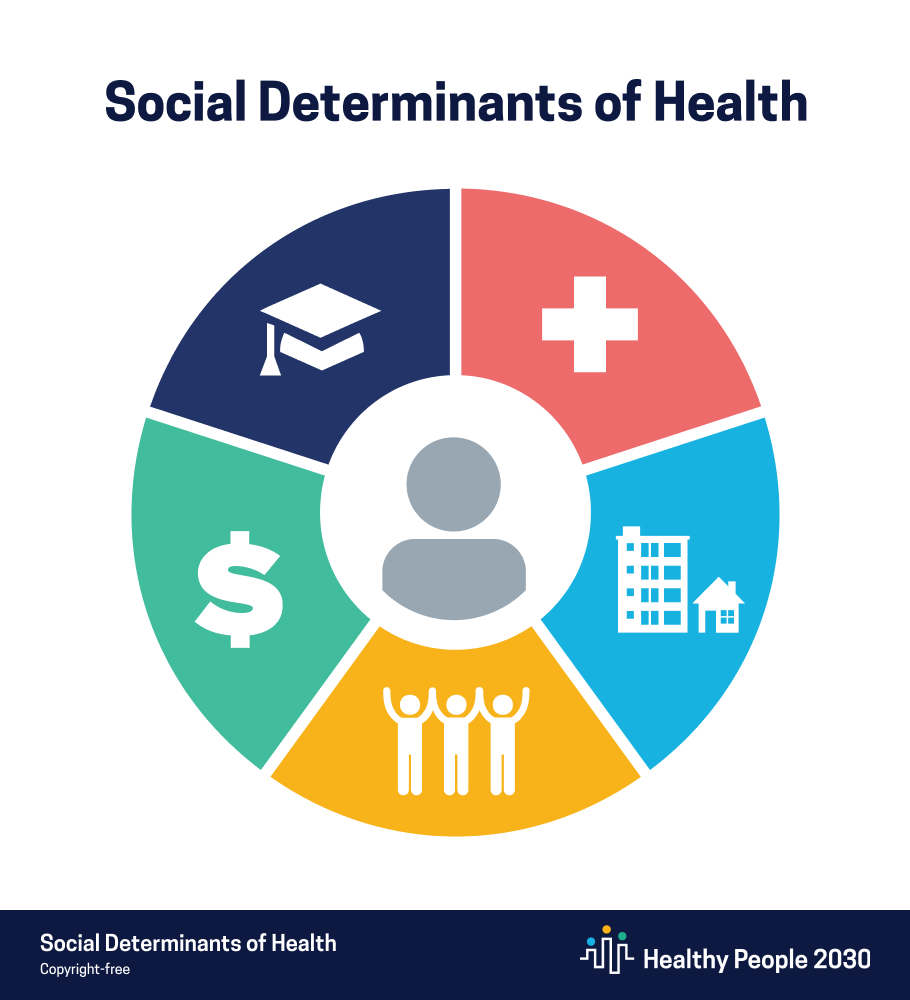
Boston Medical Center stands as a beacon of hope, recognizing healthcare can’t exist in a vacuum. Their “Thrive” program is a testament to this philosophy.Instead of solely treating ailments, they screen patients for social determinants of health (SDOH) like food, insecurity, and unstable housing, acting as navigators through a labyrinth of social services. Coming across a diabetic patient struggling with food access; “Thrive” connects them to a local food bank, ensuring their insulin isn’t rendered ineffective by an empty stomach. This holistic approach isn’t just feel-good – studies show a decrease in hospital readmissions and improved patient satisfaction, proving that addressing SDOH isn’t charity, it is smart healthcare.
Montefiore Health System
Montefiore is recognized by the U.S. News and World Report as a leader in chronic and specialty care as well as in children’s health.Language shouldn’t be a barrier to health, recognizing this, Montefiore Health System launched the “Language Access Project,” a tapestry woven with culturally competent care navigators and translated materials. Consider a Spanish-speaking grandmother worried about her grandson’s asthma, unable to navigate the complexities of the healthcare system. A “Language Access Project” navigator acts as a bridge, ensuring clear communication and culturally appropriate care, empowering both patient and provider. Montefiore Medical Center has taken great steps in implementing an interpreter services program that assists their non-English patients and their families in communicating with the medical staff.This initiative isn’t just about translation; it is about building trust and ensuring everyone feels welcome and understood within the healthcare system.
Providence Health and Services
True change requires long-term vision. Providence Health & Services understands this deeply. Their “Community Health Worker Academy” isn’t just a training program; it is an investment in the future. The Community Health Worker Academy is a collaboration between Providence and Charles R. Drew University of Medicine and Science with the goal of training people as community health workers to assist patients in clinical settings by facilitating access to care for at-risk populations.Through this academy, we can have a diverse group of healthcare leaders, reflecting the communities they serve, equipped with the skills and knowledge to champion inclusion and dismantle systemic biases. This isn’t just about ticking diversity boxes; it is about ensuring a healthcare system that understands and serves the needs of all its patients.
Children’s Healthcare of Atlanta
Similarly, Children’s Healthcare of Atlanta recognizes early intervention is key. Their Care4All children services bring primary care and preventive services directly to underserved communities.
Imagine a child in a remote rural area receiving the same quality care as their urban counterparts. This proactive approach ensures equitable access to healthcare from a young age, laying the foundation for a healthier future for all.
Norton Healthcare’s move to stop systemic racism
According to HFMA, the lack of access to healthcare services in Louisville’s underserved West End was an example of systemic racism that fueled racial and health inequities. Russell Cox the CEO of Norton Healthcare put plans in place to build a $70 million hospital in North West Louisville. Norton pledged a new focus on health equity in 2020 when they discovered how dangerous systemic racism can be.
Challenges and the Road Forward: Paving the Way with Collaboration
While these initiatives paint a hopeful picture, the road to health equity is far from smooth. Funding, ingrained biases, and community engagement remain formidable challenges. However, despair is not an option. By sharing best practices, fostering collaboration, and prioritizing long-term commitment, hospital systems can become powerful change agents.
There is the possibility of having a network of hospitals, sharing data, strategies, and resources, united in their pursuit of health equity. This collective effort can pave the way for systemic change, ensuring healthcare becomes a right, not a privilege.
The Call to Action: Building Bridges TogetherThe fight for health equity requires more than just hospital systems; it demands collective action. Here’s how you can contribute:Hold hospitals accountable: Ask your local hospital about their health equity initiatives and share your concerns.
The Call to Action: Building Bridges TogetherThe fight for health equity requires more than just hospital systems; it demands collective action. Here’s how you can contribute:Hold hospitals accountable: Ask your local hospital about their health equity initiatives and share your concerns.
Support community organizations: Donate or volunteer with organizations working towards health equity in your community.
Advocate for policy changes: Support policies that address SDOH and promote equitable access to healthcare.
Spread awareness: Share information and stories about health equity with your friends, family, and network.
Together, we can weave a tapestry of hope, bridging the gaps in access and building a healthcare system where everyone thrives, regardless of zip code, skin color, or any other social determinant. Let’s make the journey towards health equity a collective endeavor, one step, one bridge, one voiceQualify Health works with healthcare systems across the country to help solve the Health Equity crisis. These include:
Insurance payments for patients
Transportation assistance
Philanthropic solutions to patient medical bills
Charitable assistance to help patients pay their medical bills.
For more information about Patient Financial Advocacy Solutions, contact Qualify Health at (888)770-7191.